Mental Health Parity Update: 3 Key Developments in 2023
- Boutwell Fay LLP

- Apr 9, 2024
- 5 min read
Health & Welfare
Journal of Pension Benefits
Issues in Administration, Design, Funding, and Compliance
Volume 31 • Number 2 • Winter 2024
This article summarizes recent key developments in the enforcement of the requirement for mental health parity in health plans and is a follow up to a prior article that explained the basic requirements for mental health parity under the Consolidated Appropriations Act.
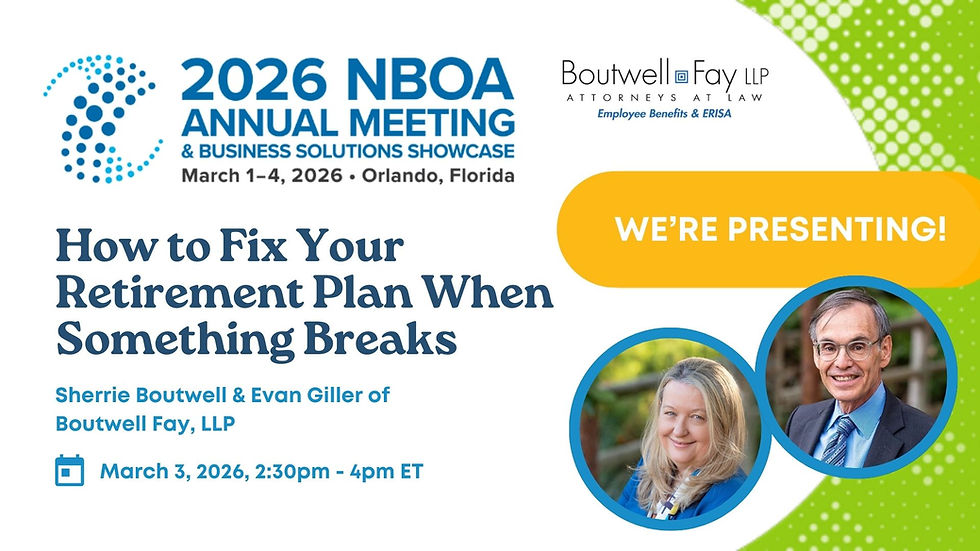
by Sherrie Boutwell, Boutwell Fay LLP
2023 saw three key developments affecting Mental Health Parity: (1) the tri-agencies tasked with enforcing that law issued extensive proposed regulations with respect to duties of plan fiduciaries under the Mental Health Parity and Addition Equity Act of 2008 (MHPAEA) [P.L. 110-343]; (2) the US Department of Labor (DOL) issued its second report to Congress regarding its enforcement activities; and (3) the courts continued to interpret and apply the law to specific cases.
Proposed Regulations
On August 3, 2023, the Internal Revenue Service (IRS); DOL, Employee Benefits Security Administration (EBSA); and Department of Health and Human Services (HHS) jointly issued new guidance in the form of proposed regulations focused on compliance with respect to non-quantitative treatment limitations under MHPEA, as amended by the Consolidated Appropriations Act (CAA) in 2021. [See https://www.federalregister.gov/documents/2023/08/03/2023-15945/requirements-related-to-the-mental-health-parity-and-addiction-equity-act]
The CAA created a new requirement for non-quantitative limitations which took effect on February 10, 2021. Under the CAA, each plan must create a written “comparative analysis” of each non-quantitative limit on mental health benefits and must provide that analysis to the DOL (or other agency with authority or a participant or beneficiary) upon request. [P.L. 116-260, Section 203] The newly proposed regulations provide extensive guidance, including new definitions and examples to help plans evaluate compliance with the non-quantitative treatment limitations (NQTL) requirements. A full discussion of the proposed regulations is beyond the scope of this column but a few notable changes include: (1) an emphasis on plans’ responsibility: although the agencies recognize that plan sponsors, administrators, and fiduciaries of self-funded health plans rarely have the expertise to properly evaluate compliance, it is still their responsibility to do it, even if they rely on third-party administrators (TPA), consultants or counsel, or contract with those parties to review compliance—so the proposed regulations require documentation of the expertise of such advisors; and (2) the proposed regulations also require a certification by one or more named fiduciaries who have reviewed the comparative analysis stating whether they found the comparative analysis to be in compliance with the content requirements of the regulations. Another notable change involves a new duty to gather and evaluate data on actual utilization of mental health services and network sufficiency.
The proposed regulations also clarify the requirements for notice—if the DOL makes a final determination of noncompliance, the plan must notify all individuals enrolled in the plan that the coverage is noncompliant with MHPAEA, which could trigger private litigation (see cases discussed below or other enforcement by the agencies).
Report to Congress
In addition to imposing burdens on plan sponsors, in the CAA, Congress also imposed a reporting requirement on the Secretaries of the Treasury Department, the DOL and HHS. At the same time it issued the new proposed regulations, the agencies also issued their second annual report to Congress about regulatory enforcement efforts.
The 2023 report is interesting in that: (1) as in the prior report, most plans do not comply, but cooperate to get into compliance; and (2) in the report, DOL shares its enforcement methodology of focusing on service providers, so if an employer becomes the subject of an investigation, it may have more to do with DOL’s concern with their service provider than with the plan itself:
EBSA is prioritizing potential violations that stem from the actions of service providers that affect not just one plan, but hundreds or thousands of plans. When EBSA finds NQTL violations in a plan, it examines the role that each of the plan’s service providers have in the design and administration of each NQTL to ascertain whether any of the service providers play a similar role serving other plans that also use the same impermissible NQTL.
During the Reporting Period, EBSA expanded an initiative targeting service providers that administer many plans for possible impermissible exclusions of key MH/SUD treatments. Under this approach, EBSA directly contacts service providers before contacting the plans they serve ... [u]nder this approach, correction first requires that the service provider change its impermissible practices, then ensures that the service provider notifies and works with all its plan clients to make necessary changes at the plan level, including amendments to plan terms, notices to participants, and payment of wrongly denied claims.
During the Reporting Period, EBSA worked with over 20 service providers using this strategic approach...These service providers collectively cover thousands of plans and millions of participants.
The comment period on the proposed regulations ended on October 2, 2023. As of this date, the Department has received 6003 comments. It is very likely that changes will be made in the final regulations once they are published.
2023 Case Law Developments
In addition to regulatory review and enforcement, MHPEA’s requirements may and are being enforced by private litigants in the courts. 2023 saw a continuation and some notable decisions in the mental health parity arena. First, the Ninth Circuit issued its most recent (and now third) decision in the ongoing saga of Wit v. United Behavioral Health [No. 20-17363, 2023 WL 5356640 (9th Cir. Aug. 22, 2023], reaffirming that the plaintiffs had standing to bring their claims and clarifying that while a court order requiring mass reprocessing of claims might be a proper equitable remedy under ERISA, the plaintiff’s had not met their burden to have that remedy in this case and sent that case back to the District Court to reconsider a number of issues including whether exhaustion of administrative remedies would be required for breach of fiduciary claims that could actually be disguised benefit claims.
In 2023, other courts have been more friendly to plaintiffs bringing actions related to mental health parity. For example, K.D. v. Anthem Blue Cross, [No. 2:21-cv-343-DAK-CMR, 2023 WL 6147729 (D. Utah Sep. 20, 2023)] in which the plan determined ongoing need for residential care ended only 16 days after treatment had begun, when the normal treatment recommendation was typically for many months; and D.K. v. United Behavioral Health, [67 F.4th 1224 (10th Cir. 2023)] in which the plan failed to meaningfully engage with patient’s providers. Another recent win for a plaintiff is M.A. v. United Healthcare Ins. [2023 BL 343110, D. Utah, No. 1:21-cv-00083, 9/28/23], which found improper denial of claim for residential “wilderness therapy.”
Conclusion
Mental Health Parity continues to be a hot topic for plans, their advisors and regulators. Look for continued enforcement, and possible expansions of these requirements in future legislation: the 2023 ERISA Advisory Council will study the impact of mental health on disability plans (mental health parity does not currently apply to disability plans). [See https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/about-us/erisa-advisory-council/2023-advisory-council-issue-statement-long-term-disability-benefits-and-mental-health-disparity.pdf].






It’s encouraging to see updates on mental health parity, since equal access to care is essential for overall well-being. These developments highlight how important it is to view health holistically—mental, physical, and preventive care all go hand in hand. In dentistry, routine dental cleaning Magnolia is a good example of preventive care that supports confidence, reduces stress, and contributes to better long-term health outcomes. Balanced care across all areas truly makes a difference.